Urinary Incontinence is the involuntary leakage of urine. In stress urinary incontinence, these leaks occur with certain physical activities such as running, laughing, sneezing or coughing. Others leak urine only when they are pregnant, after childbirth and menopause. It occurs when the bladder sphincter muscles become too weak to withhold the urine. These leaks can become frequent or severe enough to cause embarrassment and effect the social lives of women and can be treated successfully with either physiotherapy or surgery.
Some women feel the urge to urinate and cannot control it. This is called urge incontinence and is caused by overactive involuntary contractions of the bladder muscles and this can be managed effectively with medication.
The tension-free vaginal tape (TVT-O) obturator surgery is now the surgical treatment of choice for stress urinary incontinence. This surgery takes 15 minutes to perform and is done under regional or general anaesthesia. It is usually performed as a day surgery so patients can return home on the same day.
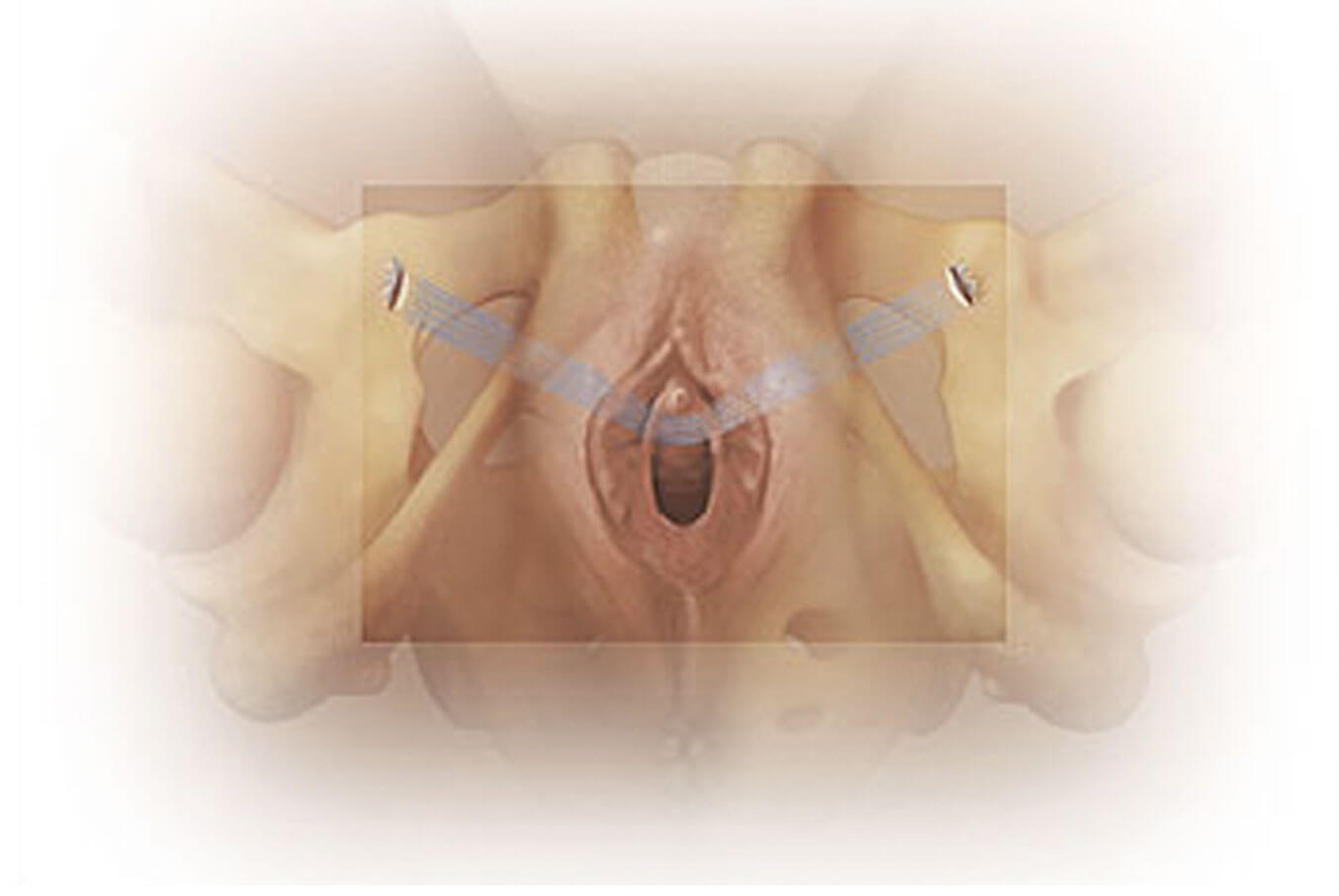
Tension-free vaginal tape (TVT-O) obturator system for Urinary Stress Incontinence
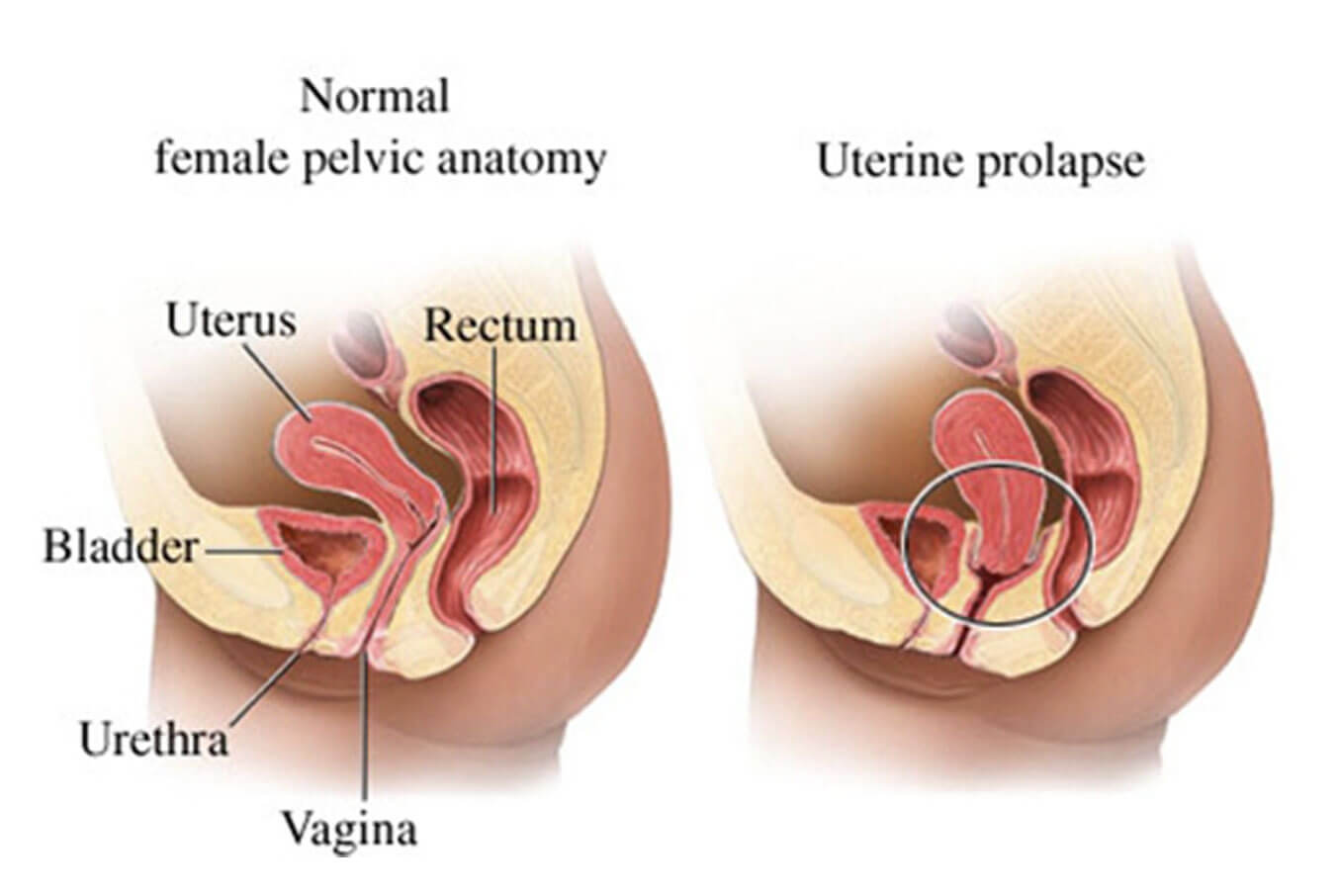
Uterine Prolapse is the condition where the pelvic floor muscles become too weak to support the uterus, resulting in the uterus descending into the vagina. It mostly affects women whose pelvic tissues have weakened because of childbirth and menopause. The loss of oestrogen and repeated straining of the pelvis eventually result in a prolapse. Treatment is usually not needed for mild cases. However, when the condition is more severe and lifestyle becomes affected, surgical repair is usually recommended by your gynaecologist in Singapore.
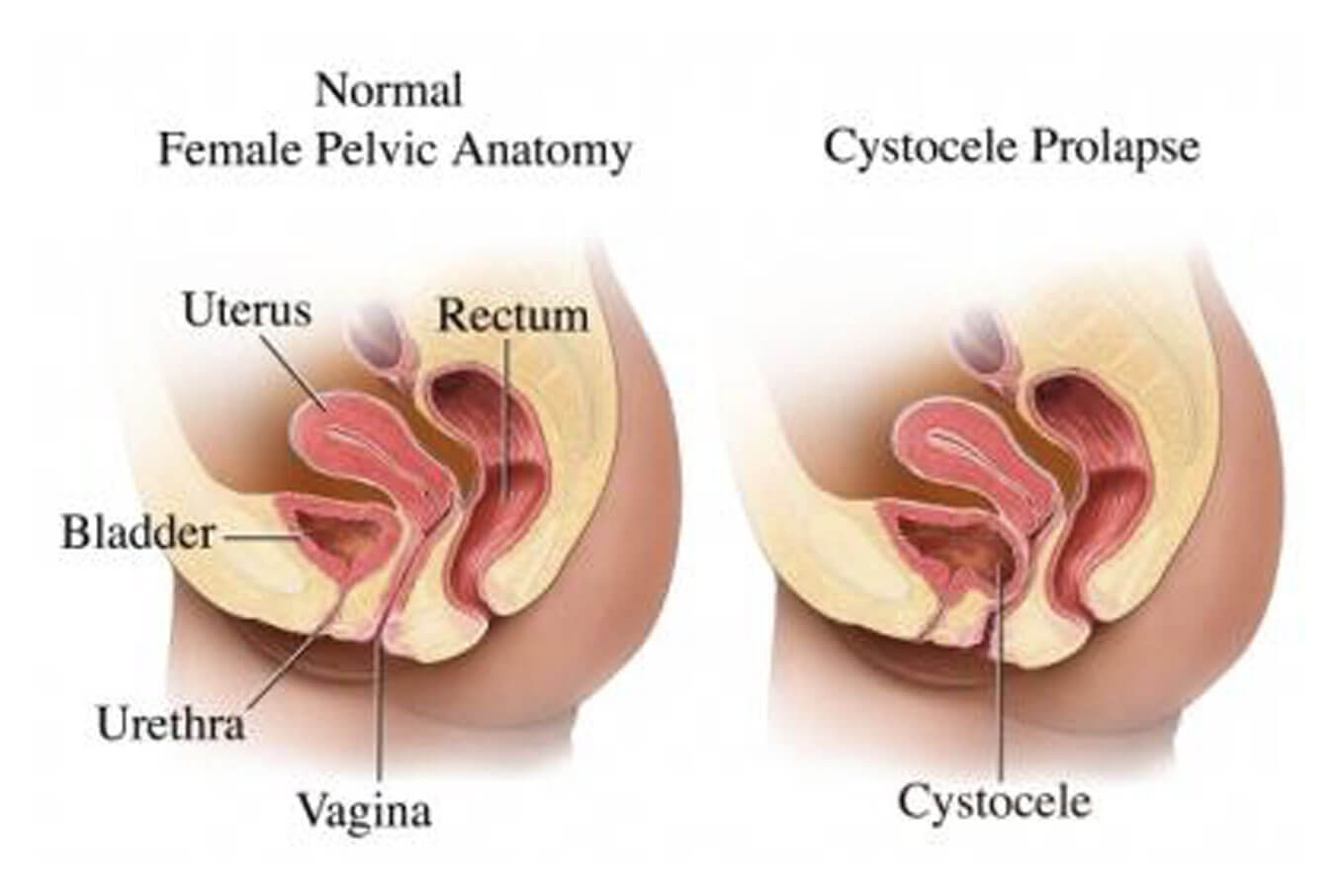
A cystocele occurs when there is a weakness of the tissue between the bladder and vagina resulting in the bladder bulging into the anterior vaginal wall. In mild cases, it can be managed conservatively but when it becomes symptomatic or the cystocele is severe, then surgical repair is warranted.
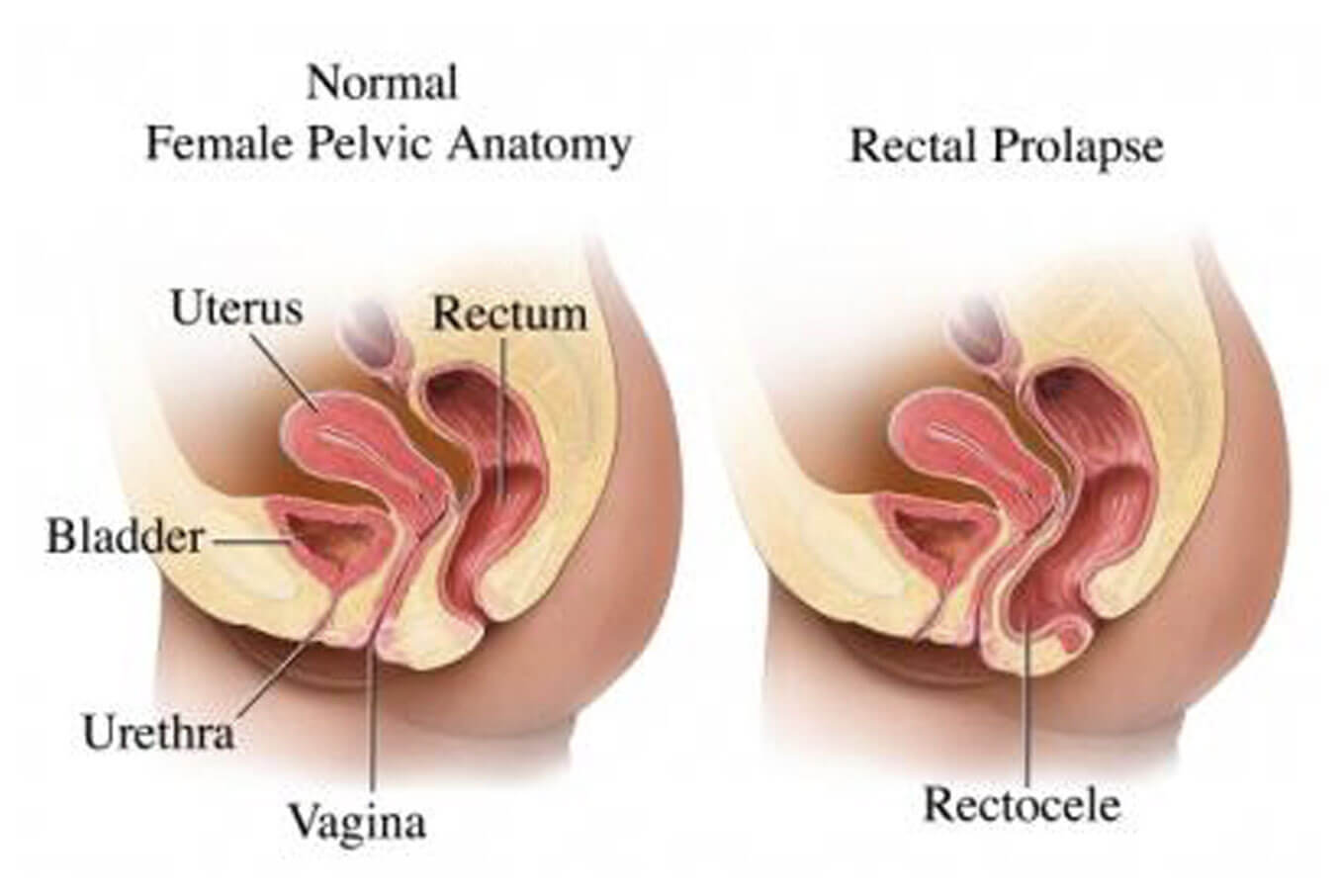
In a rectocele, defects in the tissue between the rectum and the posterior vaginal wall leads to bulging of the rectum into the vagina. Mild rectoceles do not require surgery but if the rectocele worsens and becomes bothersome or increases in severity, then surgery to repair the rectocele is usually the best method of treatment.
Both urinary incontinence and uterine prolapse can bring about distress and disruption of lifestyle. Depending on the severity, these conditions can be treated with surgery or non-surgically.
In addition, we also provide diagnostic tests and treatment for women with other related conditions like overactive bladder (passing urine too frequently), voiding dysfunction (difficulty in passing urine), recurrent urinary tract infections and other urinary symptoms e.g. pain when passing urine, blood in the urine, bed-wetting.
Some women, as a result of traumatic vaginal deliveries and/or menopause, develop lax vaginas and a gaping introitus (vaginal opening). They may start to complain of decreased vaginal tone and sensation / satisfaction during intercourse.
Vaginoplasty is a surgical procedure designed to tighten up the vaginal tissues and to reinforce tone. The normal external appearance of the vagina is restored.
The labia minora helps cushion the inner vagina and clitoris from friction, impact, and damage. Most women who are born with longer or asymmetrical labia minora have no problems and there is no cause of concern as this is part of the normal variation in appearance. For some women, however, this can cause discomfort during intercourse, frequent irritation and even ulcers during certain activities (cycling, horse riding and sexual intercourse). Others simply do not like the appearance.
Labiaplasty addresses these concerns by removing excess tissue and reshaping the labia minora to be more naturally symmetrical and functional.
Do you have questions about women’s
health and pregnancy?
Let us help you.